
Human sperm SP10 protein test kit (Immunochromatography)
Instructions for Use
For in vitro diagnostic use
CE
[INTENDED USE]
This reagent is suitable for qualitative determination of acrosomal enzyme SP10 protein in human semen in vitro. The kit can be used in assisting the diagnosis of male infertility. For professional use only.
[PACK FORMATS]
1 test/box, 2 tests/box, 5 tests/box, 10 tests/box, 20 tests/box
[INTRODUCTION]
According to the [WHO Manual of Laboratory Testing of Human Semen] (5th edition), the main factors affecting male infertility are: semen volume, total sperm, sperm concentration, liquefaction time, semen PH value, sperm normal form rate, etc., among which sperm concentration detection is an important index to measure male infertility. In this manual, the minimum normal sperm concentration is set as 15×106 sperm /ml, and when the sperm concentration is less than 15×106 sperm /ml, fertility difficulties are considered. But male infertility needs to be combined with a number of other indicators to make a final decision. Based on a number of anatomical, genetic, and biochemical characteristics, the SP10 protein proved to be a viable analyte for sperm concentration. It is only expressed in the testis and is a differentiation marker for the last step in spermatogenesis. According to the research data, the concentration of SP10 protein has a certain linear relationship with the concentration of sperm, so this reagent can be used in assisting the diagnosis of male infertility, and at the same time provide fertility guidance for appropriate age couples.
[PRINCIPLE]
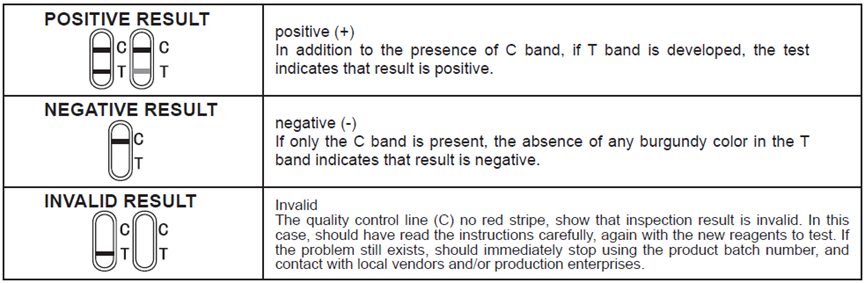
This reagent was used for qualitative determination of acrosomal enzyme SP10 protein concentration in human semen by immunochromatography. During testing, semen samples should first be processed with sample dilution, and the pre-treated sample solution is added to the sample hole. In the sample treatment solution, sperm acrosomal enzyme protein SP10 and colloidal gold labeled mouse anti-human sperm SP10 monoclonal antibody combine to form a complex, which continues to move forward due to chromatography. Form a complex with mouse anti-human sperm SP10 protein monoclonal antibody at the detection line (T-line), and a red band appears in the detection line (T-line) area, indicating a positive result. If the sample to be tested does not contain sperm SP10 protein or the sperm concentration is lower than the lower limit of the reference value, and no red band appears in the detection line (T-line) area, the result is negative. Regardless of the concentration of acrosomal protein SP10 in the sample to be measured, a red band will appear within the quality control line (C). The red band displayed in the quality control line (C) is the standard to determine whether there are enough specimens and whether the chromatographic process is normal. It also serves as the internal control standard for reagents. If no quality control line (C) appears, the experimental results are invalid.
[MATERIALS PROVIDED]
1.Test cassette
2.sample diluent buffer
3.specimen collection cup
4.specimen transfer device
5.Instruction for use
[MATERIALS REQUIRED BUT NOT PROVIDED]
Timer
[STORAGE AND STABILITY]
The kit can be stored at 4-30°C and should keep away from direct sunlight. Expiry after two years. Do not use beyond the
expiration date. After opening the sealed pouch, use the test as soon as possible within 60 minutes.
[WARNINGS AND PRECAUTIONS]
1.This test provides only a preliminary screening acrosomal enzyme SP10 protein in human semen in vitro. A confirmed diagnosis should only by a physician after all clinical and laboratory findings have been evaluated.
2.This reagent is disposable for in vitro detection and cannot be reused.
3.This reagent is not allowed to be used after expiry date, air leakage or package damage.
4.Different samples shall not be mixed, and reagent sample diluents of different batch numbers shall not be mixed.
5.Incomplete semen specimens are not suitable for semen examination.
6.Operate in strict accordance with the instruction manual, and observe and judge the reaction result within the time required by the instruction manual.
7.Do not wet the test strip or touch the reaction film before use. When used in a relatively high humidity environment, the bag should be opened for detection, to avoid high humidity environment after opening the bag for a long time to cause colloidal gold moisture absorption of reagents, resulting in deviation of the test results.
8.If the extracting solution touches eyes and mouth, a large amount of clean water should be rinsed in time and medical treatment should be sought if needed.
9.In case of any serious incident related to the device, it shall be reported to the manufacturer, distributor, EU authorized representative, notified body and the competent authority.
[SAMPLE COLLECTION]
(1) Semen should be collected in a specimen collection cup or clean plastic container, the mouth of the bottle should not be too small, otherwise, semen collection is easy to miss. Wash and dry your own container.
(2) Using artificial stimulation (masturbation) or other methods to obtain semen samples, shall not use any lubrication fluid and lotion; Or use a non-toxic condom designed specifically for semen collection, as lubricants on regular condoms, etc., may affect test results.
(3) The collection time of semen samples should be at least 2 days and no more than 7 days after the last ejaculation, during which there should be no ejaculation such as masturbation and spermatospermia. Too short or too long time will affect the accuracy of the test.
(4) All ejaculated semen shall be collected as far as possible, and shall not be omitted. If there are indeed omissions, the test results doubt, should be abstinence again as much as possible for the same number of days to collect semen for testing, the best morning semen collection. Interrupted ejaculation cannot be used for semen collection because the initial portion of ejaculation may be lost, and this portion of sperm is often the highest concentration, and inevitably mixed with vaginal secretions, affecting the accuracy of the test results.
(5) Fresh semen samples should be used for testing as far as possible (testing within 3 hours is recommended). If you want to retry later, semen samples (closed) should be stored at 2-8°C, but not more than 12 hours. Longer storage should be at -20°C and below, but only once dissolved.
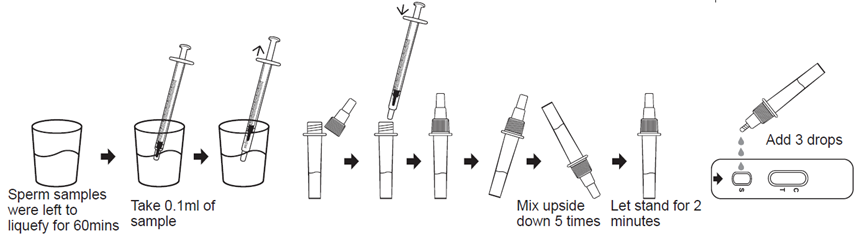
[SAMPLE PRETREATMENT]
(1) Semen will present typical semi-solid gel clumps soon after being shot into the collection container. Generally, it should be placed at room temperature for 30 to 60 minutes, and then it will be completely liquefied (that is, it will become homogeneous and relatively thin, which may contain non-liquefied gel clumps is a normal phenomenon), rarely more than 60 minutes or longer. If the liquefaction is not complete within 60 minutes, it should be considered abnormal and it is recommended to take another sample after 2 days for observation. If the liquefaction is not complete within 60 minutes, a specialist should be consulted. Only fully liquefied semen samples should be tested with this reagent. The semen sample after liquefaction must be thoroughly mixed in the original container, but not violently shaken.
(2) Use the specimen transfer device to absorb 0.1 ml of fully liquefied semen and add it to the sample diluent buffer. Note: Avoid absorbing gelatinous or sticky substances in semen.
(3) Close the bottle cap, thoroughly mix the semen and the sample diluent buffer, that is, rotate the sample treatment tube upside down for 5-10 times, if the sample is very thick or viscous, rotate it upside down again for 10 times, or stir it directly for 10-20 seconds, and then let stand for 2minutes.
[TEST PROCEDURE]
Allow test cassette, Antigen extraction buffer to equilibrate to room temperature prior to testing.
1.Open the aluminum foil bag and take out the test card.
2. Put the test card on a horizontal table, unscrew the top cap of the diluted sample, and slowly add 3 drops (about 100μL) of the pre-treated semen sample to the center of the sample hole;
3.Start timing, the reaction results should be observed within 10-15minutes, and the results are invalid after 15minutes.
[INTERPRETATION OF RESULTS]
[PERFORMANCE CHARACTERISTICS]
1. Limit of detection: sperm concentration 15×106 /ml.
2. Specificity: At the test concentration level, the following substances do not affect the test results of this reagent, they are :1x107cfu/ mL Escherichia coli,1×107 cfu/ mL Neisseria gonorrhoeae, 1×107 cfu/ mL ,Chlamydia trachomatis, 20ug/mL testosterone, 20ug/mL estradiol, and 10% whole blood, 10% saliva, 10% urine.
3. High-dose hook-like effect: When the number of sperm in the sample is no more than 3×108 /mL, there is no high-dose hook-like effect.
[LIMITATIONS]
1. This reagent is only used to assess sperm concentration in semen by detecting sperm SP10 protein, and does not reflect fertility.
2. This reagent should not be used to confirm paternity or as a contraceptive indicator.
3. This reagent is used for qualitative detection of sperm SP10 protein in the semen sample in vitro to reflect whether the sperm concentration in the sample is higher or lower than the lower limit of reference value 15×106/ml), and cannot determine the accurate sperm number in the sample.
4. The number of spermatogenesis varies greatly, so it is impossible to make a judgment based on a single test result. If an abnormal test result occurs once, samples should be collected and tested after an interval of 1 to 2 weeks. In general, samples should be rechecked for 2 to 3 times.
5. The test result is negative and does not prove infertility, since 10% of fertile men have sperm levels below the threshold. If you doubt the test result, you are advised to take a new sample for testing, and the interval between the two samples should be greater than 7 days but not more than 3 weeks. If it is still negative, it is recommended to consult a specialist at the hospital.
6. This reagent test result is positive, can not infer fertility, can only reflect the semen sample sperm concentration is not less than 15×106 /ml, because in addition to sperm concentration, a variety of factors affect infertility. Couples should consult a specialist if they have not been pregnant for a year or more while having normal sex and not using any contraception.
7. As with all diagnostic reagents, the final clinical diagnosis should not be based on a single laboratory test result, but must be made by the clinician in combination with clinical/physical and other laboratory tests.




